Guestpost: Reader B’s Experiences with an IUD
This post may contain affiliate links and Corporette® may earn commissions for purchases made through links in this post. As an Amazon Associate, I earn from qualifying purchases.
Update: We still think this is a great discussion if you're curious about other women's experiences with an IUD — but you may also want to check out our roundup of all the best birth control options right now.
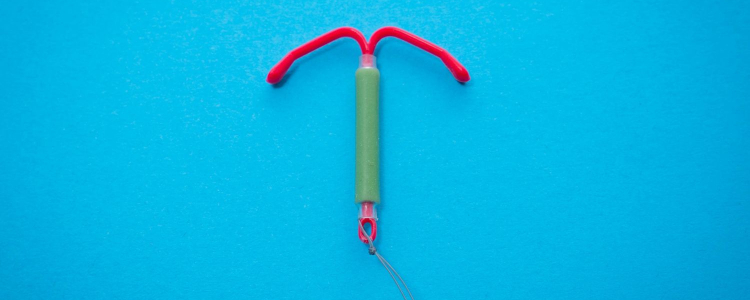
Are IUDs the right birth control method for busy women? I don't know if you've noticed, but a number of the Corporette commenters love (love) (love) their IUDs. I've never had one, but I was intrigued (particularly by their fervor!), and put out a general call for one reader to write about her experience for us. Reader B generously stepped up, and this is her account* — thank you, reader B! Let's use the comments of this post to otherwise discuss the issue. Readers, if you've had a positive or negative experiences with an IUD, please weigh in.
Reader B's Experiences with an IUD
The Decision: Why I Got an IUD
Getting a Mirena IUD was actually a relatively easy decision for me. I have had nothing but complications and woe whenever I've tried to take the pill, no matter what form of the pill I took, and I take a medicine for a chronic illness that is absolutely incompatible with pregnancy. I was in a new relationship (since ended), and given the relatively high failure rate of condoms (about 15% with typical use), I was uncomfortable using condoms alone as a method of contraception.
So I did some online research about non-hormonal methods, and went to my gynecologist intending to discuss the possibility of a diaphragm or copper IUD (brand name Paragard). I quickly discarded the idea of a diaphragm when I learned that they too have a high failure rate, but when I mentioned my heavy periods and bad PMS, my gyno suggested Mirena rather than a copper IUD.
Mirena is an IUD made of soft, flexible plastic that releases a low level of levonorgestrel, a synthetic hormone used in contraceptives. I was surprised that my gyno recommended a hormone-containing IUD, but she told me that the levonorgestrel is released only locally in your uterus/fallopian tubes/ovaries and does not spread throughout your system like the hormones in oral contraception do. For that reason, she told me that most women who have problems with other forms of oral contraception do not have problems with Mirena.
Mirena is 99.8% effective in preventing pregnancy and can remain in place for up to 5 years. If in the next 5 years I decided I wanted to get pregnant, it could easily be removed and my reproductive cycles would return to normal immediately (unlike other forms of hormonal contraception, where it can take weeks or months for a woman’s cycle to normalize after discontinuing use).
Three factors contribute to Mirena’s effectiveness. It may thicken cervical mucus to prevent sperm from entering the uterus, inhibit sperm from reaching or fertilizing the egg, and/or make the uterine lining thin. It may also stop ovulation, but the low dose of levonorgestrel is not sufficient to stop ovulation in most cases. Paragard works similarly by preventing sperm from reaching the egg, but since it is non-hormonal it does not disrupt the menstrual cycle. Although Paragard is similarly effective to Mirena and can remain in place for 10 years, I decided on Mirena because a majority of women using Mirena stop getting their periods within 3 months of insertion.
How I Prepared For My IUD (Before Insertion)
Once I decided to get a Mirena, I made a follow-up appointment for the insertion. It can’t be inserted at the same time as your annual exam; you and your doctor will need to take some specific steps to prepare for the insertion.
During my annual exam, my gyno measured my cervix to make sure I was a good candidate for an IUD. (Although there seem to be persistent rumors that only women who have given birth can get an IUD, this isn’t true; my gyno told me that it’s very rare that someone’s cervical opening is too small for an IUD to be inserted.)
The doctor’s office also wanted to pre-clear the insertion with my insurance. Perhaps most importantly, my gyno prescribed misoprostol, to soften my cervix and make insertion easier, and a muscle relaxant to reduce cramping and contractions. She also told me that I should come in when I have my period, because my cervix would be more open.
The night before the insertion, I inserted the misoprostol tablet vaginally. About an hour before the insertion, I took the muscle relaxant and 800mg of ibuprofen. Since I was a bit woozy from the muscle relaxant and I wasn’t sure if I’d be in any pain after insertion, I arranged for a friend to accompany me to my appointment.
Immediately before insertion, the medical assistant took went over some of the risks with me. The most notable was a small risk of uterine perforation; however, apparently this isn’t as bad as it sounds, because she said that in the event of perforation they’d have to stop the insertion, wait 2–3 weeks for it to heal, and then try the insertion again.
What Getting an IUD Was Like – My Experience During Insertion
I’m not going to lie; I was terrified before the insertion. I mean, they put an object in your uterus! Through your cervix! That’s gotta hurt! In retrospect, there was no reason to worry. The insertion took about 5 minutes total, the majority of which was no more uncomfortable than my annual exam. She cleaned my vaginal canal using iodine, and measured my cervix again (which felt like a sharp pinch).
When she actually inserted the IUD, it hurt badly for about 30 seconds while the insertion tool was in my cervix. I then had about 30 seconds of what I can best describe as uterine contractions. And then it was over. I didn’t have any cramping at all, probably thanks to the muscle relaxant.
I know a lot of women have horror stories about insertion. Insertion was much easier for me than it is for many women. I was very lucky to have a doctor who was aware of the possible pain and took every measure available to minimize it: the cervix softener, the muscle relaxer, the ibuprofen, and scheduling during my period. I also can’t emphasize how important it is to have insertion performed by a gynecologist who has inserted IUDs many, many times before. IUD insertion is a potentially very painful procedure with potentially difficult side effects, and it’s definitely not a procedure you want to have done by a doctor who is not experienced or not a gynecologist.
My insertion cost about $900, of which my insurance covered 80%.
How I Felt After My IUD Insertion
After insertion, I took the rest of the day off of work and slept off the muscle relaxant. I never had any cramps or contractions. My period ended a couple of days later (it is fine to use tampons with Mirena), and I experienced spotting for approximately 3 weeks. I also got a nasty yeast infection about a week after insertion. My gyno told me that this is not unheard of because the insertion can change the pH level in your vagina, but that it was also possible that the yeast infection was unrelated to the Mirena.
I had a follow-up appointment 4 weeks after the Mirena was inserted. My gyno checked to make sure that the Mirena was still in place and that I wasn’t having any complications. Going forward, she told me to check monthly to make sure the strings are in place by feeling my cervix. Other than that, I don’t have to think about birth control at all.
There are some complications that can develop immediately after insertion, including severe cramps and even expulsion of the IUD. In the longer term, less than 10% of women experience minor side effects, and there are some potentially serious but extremely rare complications that can occur including infection or embedment in the uterine wall (the same complications can occur with the Paragard IUD). My gyno discussed these risks with me before I decided to have Mirena inserted.
Sex with the IUD is pretty much the same as sex before the IUD. I can’t feel it inside me, and my partner can’t feel it either. It has no effect on my libido or ability to get aroused. I have read that some men can feel the strings, but in that event your gyno can trim them.
Mirena does not protect against STDs, so I still use condoms since I’m not in a monogamous relationship with a trusted partner. I’ve had no side effects, and my periods have gone from 6 days of heavy bleeding to 1–2 days of very minimal spotting. Overall, I’m extremely happy with my decision to get an IUD, and I will definitely get another one if I don’t want kids when my 5 years are up.
* Reader B has no affiliation with Mirena. I have not extensively fact-checked her post; please ask your doctor any specific questions, particularly whether an IUD is right for you. In general, this is not intended to be an advertisement or endorsement for any particular brand or type of birth control (or medical advice of any kind) — just a discussion among friends (similar to the guest post from my friend who froze her eggs). – Kat.
Readers, have you had positive or negative experiences with an IUD? Which birth control form do you prefer?
Further reading:

Hello, I think your web site might be having web browser compatibility problems.
When I look at your web site in Safari, it looks fine however when opening in IE,
it’s got some overlapping issues. I merely wanted to give you a quick heads up! Apart from that, great website!